In 2018 global health expert Jonathan D Quick, of Duke University in North Carolina, published a book titled The End of Epidemics: The Looming Threat to Humanity and How to Stop It. In it he prescribed measures by which the world could protect itself against devastating disease outbreaks of the likes of the 1918 flu, which killed millions and set humanity back decades. He is the former chair of the Global Health Council and a long-term collaborator of the World Health Organisation (WHO).
The Covid-19 epidemic looks like it’s edging towards becoming a pandemic — that is, as the WHO defines it, “the worldwide spread of a new disease” — but the WHO hasn’t declared a pandemic yet. What are the best-case and worst-case scenarios?
The best case is that the Chinese conflagration is brought under control, the smaller “flames” we’ve seen flare up in other countries are extinguished, there’s little or no spread to new countries or continents, and the epidemic dies out. The worst case is that the outbreak goes global and the disease eventually becomes endemic, meaning it circulates permanently in the human population.
Your feeling as to which is more likely, as of today?
The worst-case scenario is looking increasingly likely. We’ve now seen cases on six continents, apparently “silent” — that is, at least partly asymptomatic — chains of human-to-human transmission both inside and outside China, with additional countries reporting cases within the last week — bringing the total to 47 — and new, accelerating outbreaks in Iran, Italy and South Korea. If it becomes a pandemic, the questions are, how bad will it get and how long will it last? The case fatality rate — the proportion of cases that are fatal — has been just over 2%, much less than it was for Sars, but 20 times that of seasonal flu. There are still many unknowns — we may have underestimated the period during which a person is contagious, for instance, and the variety of ways in which the virus spreads.
If the worst-case scenario comes true, are there still things we can do to minimise the pandemic’s impact?
Absolutely. We can mobilise more health officials and keep engaging the public, implementing sensible travel controls and ensuring that frontline health workers have ready access to diagnostic tests and are vigilant — that they don’t send anyone who may have been exposed home without testing them, for example. Judging by past experience, however, it’s likely that health officials and the public in much of the world remain unaware or unconvinced of the danger this virus poses.
You have said that time and trust are critical to good epidemic management. What do you mean?
The delay between the frontline health workers noticing something unusual, in the form of an emerging disease, and that information travelling up the line to central decision-makers is critical. To illustrate that, a 2018 simulation that the Gates Foundation conducted of a flu pandemic estimated that there would be 28,000 after one month, 10 million after three months, and 33 million after six months. The virus used in that simulation was more contagious and deadly than Covid-19 — though they are both respiratory viruses — but the example shows how all epidemics grow exponentially. So if you can catch an epidemic in the first few weeks, it makes all the difference. As for trust, it’s critical to disseminate dispassionate, evidence-based information, and not to try to mislead the population. If you do, they will stop co-operating. Let’s hope that doesn’t happen in China.
Judging by reports, we’re at least a year out from having an approved Covid-19 vaccine. Once one is available, do you think there will be a problem of vaccine hesitancy, as there has been with some of the resurgent childhood diseases?
Evidence suggests that vaccine hesitancy diminishes when lots of people are dying. Once an outbreak is over, however, levels of vaccine uptake may depend on how fresh that outbreak is in people’s minds — even though the risk of another one is real. I’ve written about a hypothetical situation in which a new and dangerous pathogen emerges, a vaccine is developed, and you still get a pandemic, because large numbers of millennials refuse the vaccine. In the US, 20% of millennials believe that vaccines cause autism. The problem is bad information. As my students often remind me, news tends to be behind paywalls, while fake news is free.
Is it plausible that the Chinese have already created a Covid-19 vaccine?
The US drug company Moderna is the only one I’m aware of that has a Covid-19 vaccine ready for human trials. Those are due to start in April. Chinese firms are new to the global vaccine market, but at least one, Clover Biopharmaceuticals, is working to develop a Covid-19 vaccine.
It appears that the Covid-19 virus originated in a “wet” or live animal market. Should such markets be banned?
No. The Chinese government tried that after Sars. The markets just went underground. They need to be better regulated, and there needs to be active surveillance. Active monitoring and culling of poultry populations in Asia has stamped out outbreaks of avian flu in those populations.
Was an epidemic like that of Covid-19 inevitable?
From a biological standpoint an outbreak of a novel pathogen was inevitable, but this one happened in the worst place at the worst time. Wuhan is a big city and a crossroads, and the first cases were recorded there just before the lunar new year, when large numbers of people were about to travel to visit their families.
In terms of containing it, was it a good or a bad thing that it happened in China?
As of five months ago, we have a measure of epidemic preparedness — the Global Health Security (GHS) Index — that scores countries on six dimensions: prevention, detection, response, health system, risk environment and compliance with international standards. No country scores perfectly on all six. China has detected and responded to this epidemic pretty well, though its health system is now stretched beyond capacity, but it is weak on prevention — particularly when it comes to food safety.
How well is the US prepared?
The US ranks high on the GHS index, but is still unprepared for a severe pandemic, should one happen. Malfunctioning coronavirus tests have frustrated public health labs and delayed outbreak monitoring. Supplies of masks, suits and other protective material for health workers are running low in the midst of a moderately severe flu season. Since the creation of a much-needed public health emergency preparedness fund in the aftermath of 9/11, its budget and the public health functions it supports have been steadily reduced. This is the mentality that left the world vulnerable to the devastating 2014 outbreak of Ebola in west Africa — that is, close the fire department and cancel the fire insurance as nobody’s house or factory has burned down lately. It’s time we learned that the bugs never stop mutating and crossing over to humans.
Has the world been an ostrich over pandemic risk?
Generally speaking, no. After each major recent outbreak — Sars, swine flu, Ebola — we’ve moved ahead. The GHS Index is itself a big advance, because we can now see where individual countries are weak in terms of preparedness. We should be moving faster, though.
What exactly should we be doing faster?
Fewer than one in three countries are close to being prepared to confront an epidemic, which leaves the vast majority of the world’s population vulnerable. That in turn leaves us all vulnerable because we’re only as safe as the least safe place. We need to invest more in preparedness, and we need our leaders to take a greater interest in it — that’s all leaders, in both the public and private sectors — from the grass roots to the grass tops.
Is a global health agency essential to managing a pandemic, and is the WHO up to the task?
A global health agency is essential, yes. None of the advances I’ve mentioned could have happened without the WHO’s involvement, but the WHO can only perform as well as its members allow it to — and they have pulled back on funding since the 2008 financial crisis.
Your book is optimistically entitled The End of Epidemics. Could we ever really wave goodbye to epidemics?
The world will continue to have disease outbreaks, but there is plenty we can do to protect ourselves against global catastrophes like the 1918 flu. — The Guardian
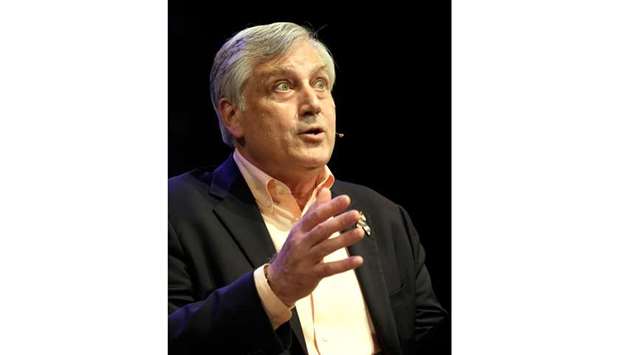
FIRST LESSON: u201cIt’s critical to disseminate dispassionate, evidence-based information, and not to try to mislead the population,u201d says Jonathan Quick.
